We are all ready to say goodbye to the COVID-19 pandemic. The past few years have been arduous, exacting a terrible toll in human suffering, economic turmoil, and political strife. More than 1 million Americans perished, as did a sense of well-being for our health and mental wellness. And while the SARS-CoV-2 virus will likely persist among us for a very long time, it appears that the worst is over, thanks to modern medicine and public health prevention.
We have come through the other side of the worst pandemic in a century intact and better prepared than before.
Colorado State University’s contributions have been invaluable. New connections were quickly made among faculty, community partners, and industry that allowed for a quick pivot to innovative approaches to slow the rapidly spreading threat of COVID-19. These efforts included testing the efficacy of face masks, creating diagnostic and screening methods, quantifying aerosols to better understand the spread of the virus, developing approaches to surveillance among skilled nursing facility workers and residents, wastewater surveillance, and vaccine development. In addition, we responded to the repercussions of isolation, including declines in mental health and increased loneliness. Among these innovations was the development of wastewater testing for SARS-CoV-2, technology that provided our campus and community an early-warning surveillance system to track the virus before most people even knew they were exposed. Mandatory testing for COVID-19 was conducted in areas that saw high wastewater levels of the virus, allowing those who tested positive or were exposed to isolate or quarantine before infecting others. This system also gave our local health department valuable information that helped to minimize community spread.

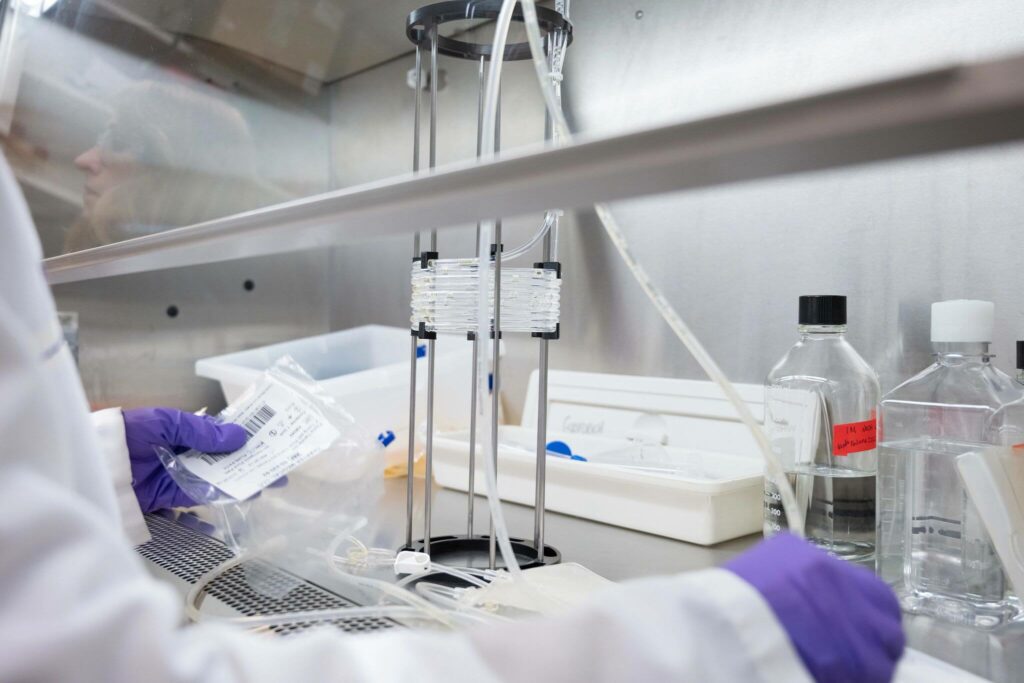
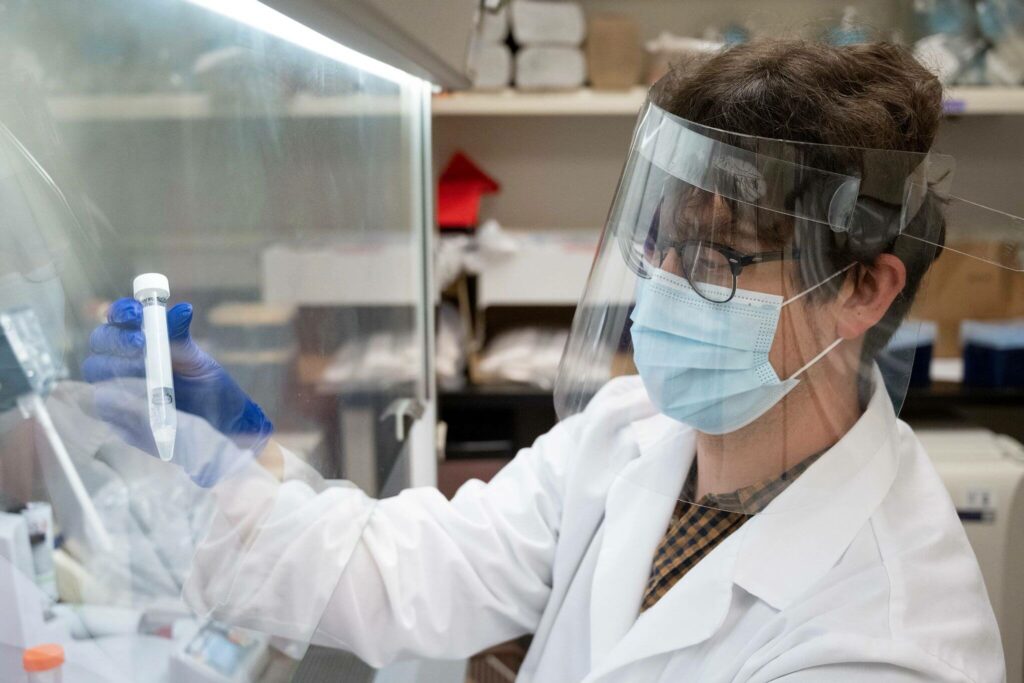
Susan De Long, associate professor of civil and environmental engineering, and students Nicholas Mohammed and Thomas Anderson sample wastewater from one of 17 collection sites on campus to be tested for the COVID-19 virus. Credit: John Eisele, CSU PhotographyIn addition, CSU began work to prevent future cases through development of SolaVAX™, a COVID-19 vaccine candidate. SolaVAX™ is a process that uses ultraviolet light and riboflavin (vitamin B2) to create an inactivated virus, which can safely stimulate a person’s immune system, similar to the flu vaccine. The National Institutes of Health awarded the team a base contract worth $3.1 million to continue to develop the SolaVAX™ process that will not only help fight future coronaviruses but also other emerging pathogens. Another technology that quickly followed was the development of VacciRAPTOR, a photochemical reactor that can inactivate many types of viruses and pathogens more efficiently than past systems. This technology has increased CSU’s capability to create and test vaccines, allowing a faster path toward clinical trials.


Slowing the spread of COVID-19 was only part of the solution; the pandemic was also having devastating effects on our mental health. The pandemic left many people alone for extended periods of time, without social connections and distanced from family and friends. CSU faculty and community partners were quick to intervene with the development of THRIVE, a support service for older adults offered through the Columbine Health Systems Center for Healthy Aging that includes virtual and telehealth services. Participants were matched with a CSU student who introduced them to different services ranging from technology assistance to exercise and wellness activities, nutrition counseling, music connections, respite care, pet interactions, and social support groups. The program lasted eight weeks with the opportunity for participants to continue in the program through a care coordinator. There were lots of success stories from this project for both the older participants as well as the students.
At the same time, we also witnessed the limitations and flaws in national systems including failures in coordinated communication allowing misinformation to spread as fast as the virus itself, leading to a breakdown in trust of the public health system at all levels. Health inequities were amplified during the pandemic when we saw higher death rates and less access to preventive measures among the most vulnerable communities.
According to the Centers for Disease Control and Prevention, Hispanic/Latino, African American, and American Indian and Alaska natives had 1.5, 1.1, and 1.6 times respectively greater likelihood of getting COVID-19 than their white, non-Hispanic counterparts. Further, they had 1.7, 1.6, and 2.0 times respectively greater likelihood of death from COVID-19 than their white, non-Hispanic counterparts. Importantly, race and ethnicity are markers for other underlying conditions that affect health, including socioeconomic status, access to health care, and exposure, as many of our frontline, essential workers came from these racial/ethnic groups. Such inequalities need to be addressed to battle any future pandemic effectively and justly.
So where do we go from here? How will we better prepare for the next disease outbreak?
To start, we will need to continue to be innovative in how we consider future coronavirus outbreaks as well as how we consider potential new pathogens that result from climate change. We are already making inroads in these areas with The Anschutz Foundation contribution to CSU in the form of nearly $2 million for pandemic-related research projects and graduate fellowship research programs that will help us confront present and future infectious disease threats among animals and people. Also, CSU faculty recently received $12.5 million from the National Science Foundation to study the air microbiome. Called the Biology Integration Institute Regional One Health Aerobiome Discovery Network, or BROADN, it aims to gain a better understanding of how the air is altered by environmental stressors and how this impacts human, animal, and environmental health.
Future work will also need to address how we communicate science and how we coordinate this communication. We will also need to continue to strengthen our engaged community work to build trust in science and public health research as well as address health inequalities. Not surprisingly, CSU administration and faculty are already tackling these issues. Health communication faculty are currently designing courses that focus on new and innovative ways to communicate science and risk. The Office of Extension and Engagement is also building on our land-grant mission “to improve the quality of life for people in all communities” by putting more resources toward engaged scholarship, allowing our faculty dedicated time and support to better engage with communities. Meanwhile, the Rural Initiative is placing Extension health and behavioral health specialists throughout the state to engage with communities and help them tackle the local health issues they face. Such community collaborations and connections will help establish trust in our institutions that work on health-related issues.
We are also looking ahead to training future public health practitioners with the establishment of an academic health department partnership with the Larimer County Department of Health and Environment. Similar to what the teaching hospital is to a medical school, this partnership will allow us to enhance public health education, training, research, and service, strengthening the links between public health practice and academia.
It is clear the COVID-19 pandemic revealed strengths and weaknesses among all sectors of society. For CSU, we saw our strengths shine and resiliency revealed. Faculty came together in unprecedented ways, developing partnerships that will have long-lasting effects. We also saw new community partnerships develop and current ones strengthened. Most importantly, all of these partnerships and initiatives were, and continue to be, conducted through the lens of our CSU Principles of Community: inclusion, integrity, respect, service, and social justice, which in the end will impact health equity – giving everyone a fair and just opportunity to attain their highest level of health.
Tracy Nelson is the director of the Colorado School of Public Health and a professor in the College of Health and Human Sciences at Colorado State University.